@2021 invictIQ is a venture by Sprint Consultancy. All rights reserved. Privacy Policy.

Documentation and Best Practice for Record Keeping
by Mark Topps
We all know the famous saying in social care ‘if it’s not documented, it didn’t happen’ and this has underpinned a golden thread for generations of care workers to ensure robust record keeping. I am always conscious that I have experienced managers follow my content, but also a number of newer managers into the sector, and don’t ask me why, but I feel a sense of responsibility to ensure our next generation of Registered Managers have tools and insight to grow and be successful in their role. There are many great resources shared these days into the sector which is great, and I thought I would go semi-back to basics to understand the purpose of documentation, how audits can help (after all, this blog is in partnership with InvictIQ) and some common pitfalls that are made within the sector.
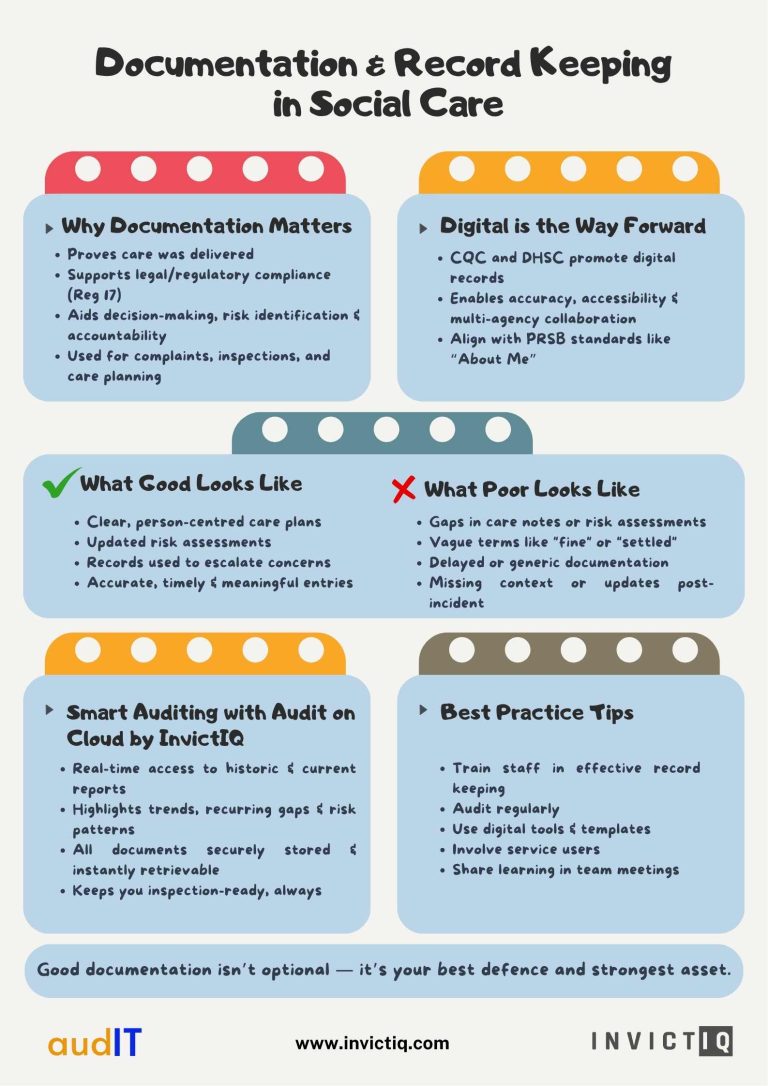
Why Documentation Matters
The short answer is that documentation is your evidence! Slightly longer answer is that documentation is much more than just an account, it’s the foundations for so much more, it is the centre of how you demonstrate the care you are delivering, how you are meeting people’s needs, a timeline of care decisions and interventions you and your team have made, the impact you are having, be the evidence to push back on complaints, the tool to help identify risks and areas for improvement.
Good record keeping also isn’t a nice to have, it’s a legal responsibility for providers. Under Regulation 17 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014, providers must maintain accurate, complete and contemporaneous records. This regulation is often cited in inspection reports where services fall short.
The CQC expects providers to:
- Assess, monitor and improve the quality and safety of services.
- Maintain secure and accessible records for each service user.
- Use records to inform decision making and support learning.
Failure to meet Regulation 17 is one of the most common reasons for a service being rated as “Requires Improvement” or “Inadequate”.
The Digital Era of Record Keeping
The majority of services are now keeping their records digitally, and for those who are not yet doing so, the CQC and the Department of Health and Social Care are increasingly encouraging the use of digital, citing the key benefits of data accuracy and accessibility, real-time updates, reduction of duplication and to support multi-agency collaboration and continuity of care.
One body I only found out about a little while ago was the Professional Record Standards Body (PRSB) who have developed national standards for digital records, including the “About Me” standard, which supports personalised care planning and is linked in with the CQC expectations under their best practice and guidance signposting. You can read more here: Sources of best practice and guidance – Care Quality Commission
What does Good and Poor Recording Keeping Look Like and the Role of Auditing
Feedback from CQC inspectors and peer audits often highlights the quality of documentation as a key differentiator between “Good” and “Outstanding” services. Common themes include:
- Clear, person-centred care plans that reflect the individual’s voice.
- Risk assessments that are regularly reviewed and updated.
- Evidence of staff using records to inform care and escalate concerns.
Poor record keeping is more common in some of the CQC reports, with these being some of the common themes:
- Gaps in care notes
- Missing risk assessments
- Unsigned care plans.
- Lack of person-centred detail (generic care plans that don’t reflect the individual’s preferences, history or needs) which could breach Regulation 9 (Person-centred care).
- Delayed record peeping (notes written hours or days after care was delivered)
- Using vague terms like “settled” or “fine” without context.
- Using abbreviations which can be misunderstood and misinterpreted.
- Poor record security or confidentiality which could break Regulation 17.
- Lack of evidence for decision making such as why a medication was withheld or why a safeguarding referral was made.
- Impact: Weakens accountability and can lead to regulatory action.
- Lack of evidence for decision making or family involvement
- Records not updated following incidents or changes in need.
From my experience mock inspections and audits help ensure that care plans are person-centred, regularly updated and are reflective of individual needs and preferences. They also highlight gaps or inconsistencies that may indicate training needs or reviews to take place. Beyond compliance, audits promote a culture of continuous improvement and you should build this into supervisions and team meetings so your team are aware of the importance of strong record keeping.
Audit on Cloud by InvictIQ makes this process even easier by allowing instant access to historic and ongoing reports, making patterns of repeated errors or gaps easier to spot and address. Documents are securely stored and effortlessly retrievable, helping services stay responsive, consistent and ready for inspection at all times.
Best Practice Tips for Providers
- Train staff on the importance of documentation and how to record effectively.
- Audit records regularly to ensure consistency and completeness.
- Use templates and prompts to guide staff in capturing key information.
- Involve service users in their care planning and documentation.
- Embrace digital tools that align with national standards and improve efficiency.
Remember, if it’s not written down, it didn’t happen.

Mark Topps is a social care leader who has worked in the care industry since 2004 and is currently working as a regional support manager. He regularly advocates, appearing on television, radio and podcasts and has started many campaigns for change in legislation and culture within the industry. Mark is the co-founder of The Caring View which is a social care podcast, YouTube show and free resource initiative for the sector. He also co-founded The Health and Social Care Club, which is an audio event hosted on LinkedIn. Mark is also the social media and marketing director at the National Association of Care and Support Workers.
Sign up for our newsletter