With the upcoming changes to the way the CQC regulate, I thought it would be a good time to stop, reflect on the changes that are being made and look at what the regulator is looking for.
What changes are happening?
Historically inspections have been face-to-face, with an inspector visiting you and going through records and documentation, however as we move into the digital way of working, the CQC are doing away the same. Inspections are more than likely to be remote and the CQC have stated that the PIR is still an important part of the information gathering process, and the new provider portal will make it easier to collate information from providers, NHS England, Local Authorities and other sources. This data will create a more real time view of the service and allow the inspector to make an informed decision to the outcome of the inspection.
The CQC will keep their current inspection ratings, however unlike at the moment where you could go a couple of years without an inspection, due to being data led, inspections will take place more frequently, although the CQC have not stated how often this will be. The current inspection ratings are:
- Outstanding
- Good
- Requires Improvement
- Inadequate
Inspection outcomes will still be in a report, however to compliment this there will be new benchmarking tools used on the CQC website, so that providers can see where they sit compared to other services, both at a local and national level.
Whilst the CQC will retain the Safe, Effective, Well-Led, Responsive and Caring key questions, they will be implementing 5 to 8 quality statements under each heading.
I / We statements are being introduced, so that people using care services are put at the heart of all we do. I statements are about what good care looks like from the person drawing on care and the We statement is how the organisation is going to meet those needs.
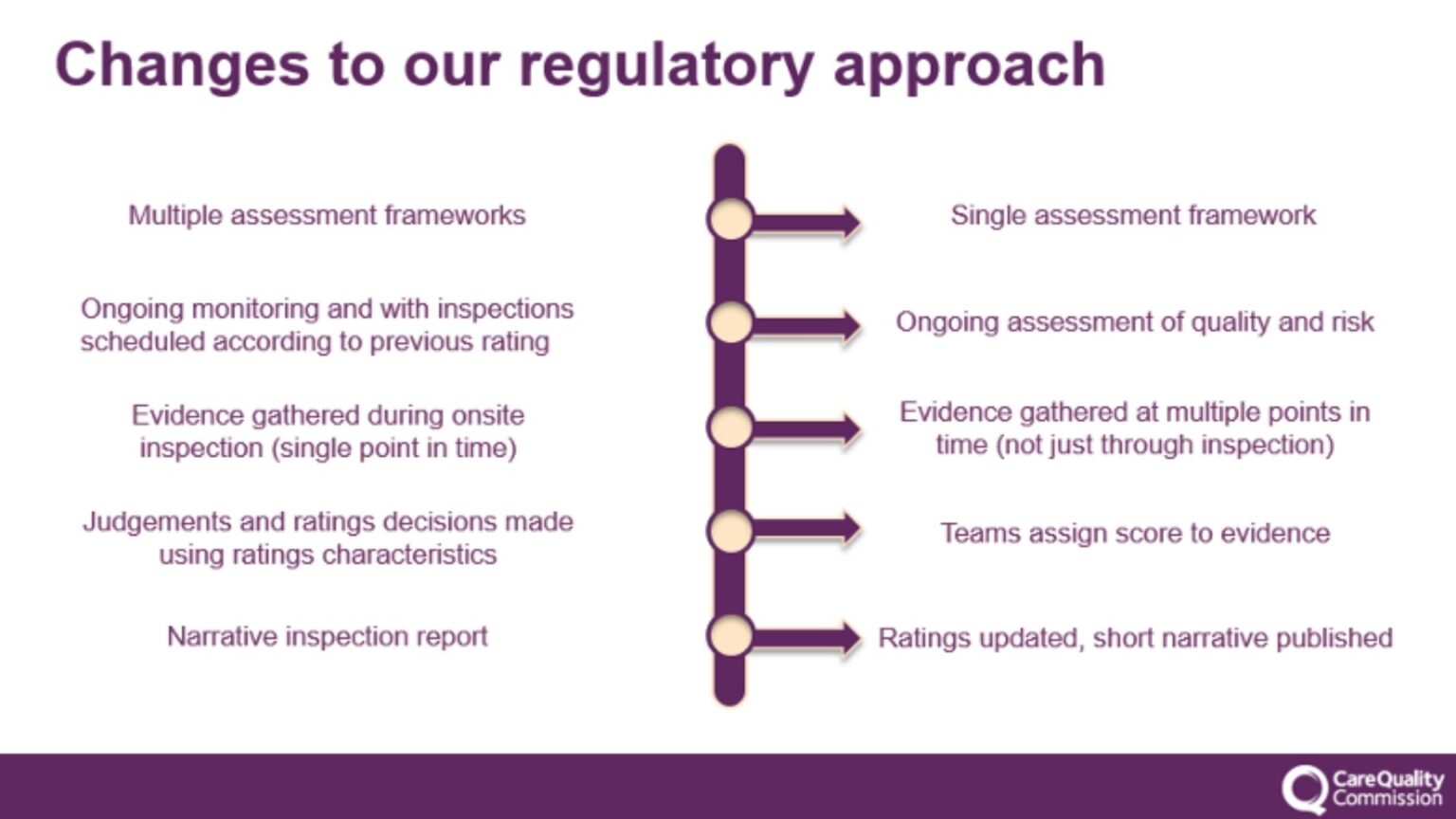
The CQC is hosting a number of webinars, so make sure you register for their newsletters to stay up to date with their changes. The visual below shows how they are changing their approach.
What the regulator is looking for.
The regulator will know the providers cannot implement changes overnight, however they will want to be reassured you know what the changes are and have a roadmap to outline the changes you will be making in your service.
Remember the five key questions that the CQC will ask: Safe, Effective, Caring, Responsive and Well-Led. The easiest way I learnt how to remember them all was with the acronym SCREW.
Safe
Caring
Responsive
Effective
Well-Led
When looking at those five key questions, they will want evidence you are meeting them. Here are some insights:
Safe
Inspectors check whether the service is safe for the people using them and this will include monitoring infection control measures, medication management, safe and effective staffing, a visual check of the environment to make sure it is safe, policies and procedures, positive risk taking, that equipment is serviced and in good repair, safeguarding records and a culture built on learning.
Health and Safety and Infection Control remain hot topics, and you should ensure you are auditing your services on a regular basis, with actions being dealt with in a timely manner. The regulator will want reassurance that you have systems in place to learn from incidents/accidents, how you learnt from them and the steps you are putting in place to reduce or stop them from happening again in the future.
Health and Safety includes risk assessments, fire safety and infection prevention measures.
Effective
The inspector will check goals and aspirations of those using the care service vs how the care provider is achieving these. They will also check how teams work together, how people are supported to live healthier lives, training matrix/records, induction plans, care plans and risk assessments built on consent and being person led.
The regulator does not stipulate what training you should be providing to your teams or how frequently this should be provided. Historically they have stated ‘providers must deploy sufficient numbers of suitably qualified, competent, skilled and experienced staff to make sure that they can meet people’s care and treatment needs.
You should ensure you keep a up to date training matrix and be able to evidence how you support staff with ongoing training, developmental support and how you as a provider stays up to date with the latest regulations and practices. You can read the full guidance here.
Caring
Inspectors look at whether the care provided is compassionate and respects the dignity and privacy of those using the service. They will look at how staff communicate with each other and those being supported, how staff respond to questions and/or requests from people, that people are treated as individuals, that independence, choice and control underpin good care outcomes, that MCA/DoLS records are in place and that person centred care is in place and that the provider has the best interest of the person at the heart of all they do.
A new element within the inspection will be around workforce wellbeing and an enablement ethos.
Responsive
This aspect of inspection assesses whether services are responsive to the individual needs of people. It looks at how well services adapt to the changing needs of individuals, that people are provided information, listened to and involved, whether there is a mechanism for receiving and addressing complaints and feedback, that there is equity in access and outcomes and that the service plans for the future.
Care plans should be reviewed and updated as and when there are any changes, or at least on a regular basis to ensure that the care and support being provided meets the needs of the individual and is being given in a way that the person would like to receive. Evidencing reviews and quick responses to changes in care needs will evidence to the regulator that you are responsive and effective to people’s needs and preferences.
Audit care notes and ensure they are detailed, factual and legible. Address areas of concern and upskill staff where needed. Care notes are your evidence of the care being delivered and can help demonstrate what your team are doing if an inspection checks the notes.
Well-led
CQC inspectors want reassurance that managers and senior teams have oversight of the service. Inspectors will want to see a shared direction and positive culture, compassionate and capable leaders within the organisation, action plans, policies and procedures, lessons learnt, evidence of continuous improvement and a copy of any recent complaints. Services should stive to create workplaces where people can speak up, that are inclusive, diverse and offer equality to those who work and live in the service. The CQC will also be looking for services to be environmentally sustainable.
Final Thoughts
We all know that our brain goes out the window when the inspector calls, so ensure you capture success stories, events that have had a positive impact on someone’s life, case studies etc throughout the months as these are all great things to have to hand during an inspection. The regulator is keen to see the positive impact on people and their lives, so make sure you and your teams can demonstrate this. In this regard, platform like audIT On Cloud by InvictIQ comes handy. It is an easy-to-use, one-stop solution for managing all your audit, inspection and complaints, making your Care businesses compliance ready always. Not only are all actions, evidence and reports centralised in the cloud, their dashboard empowers providers with real-time data insights, enabling effective storytelling.
I hope the above has helped you prepare for what the regulator is looking for but make sure you also upskill your teams about the inspection process during team meetings and in day to day conversations. Break down the stigma of the CQC being scary people and embrace them as people who come to provide feedback and enhance the quality of care where it may not meet expectations. We can all improve, and this is part of that continuous loop of improvement planning.