I was recently contacted by a manager who has been asked to go to one of the company’s sister homes and review the processes in place, following a requires improvement outcome on their inspection. We discussed many things from care plans to risk assessments, from food hygiene to infection control but one thing we spent time talking about, and one thing we kept coming back to was audits, and the importance of these.
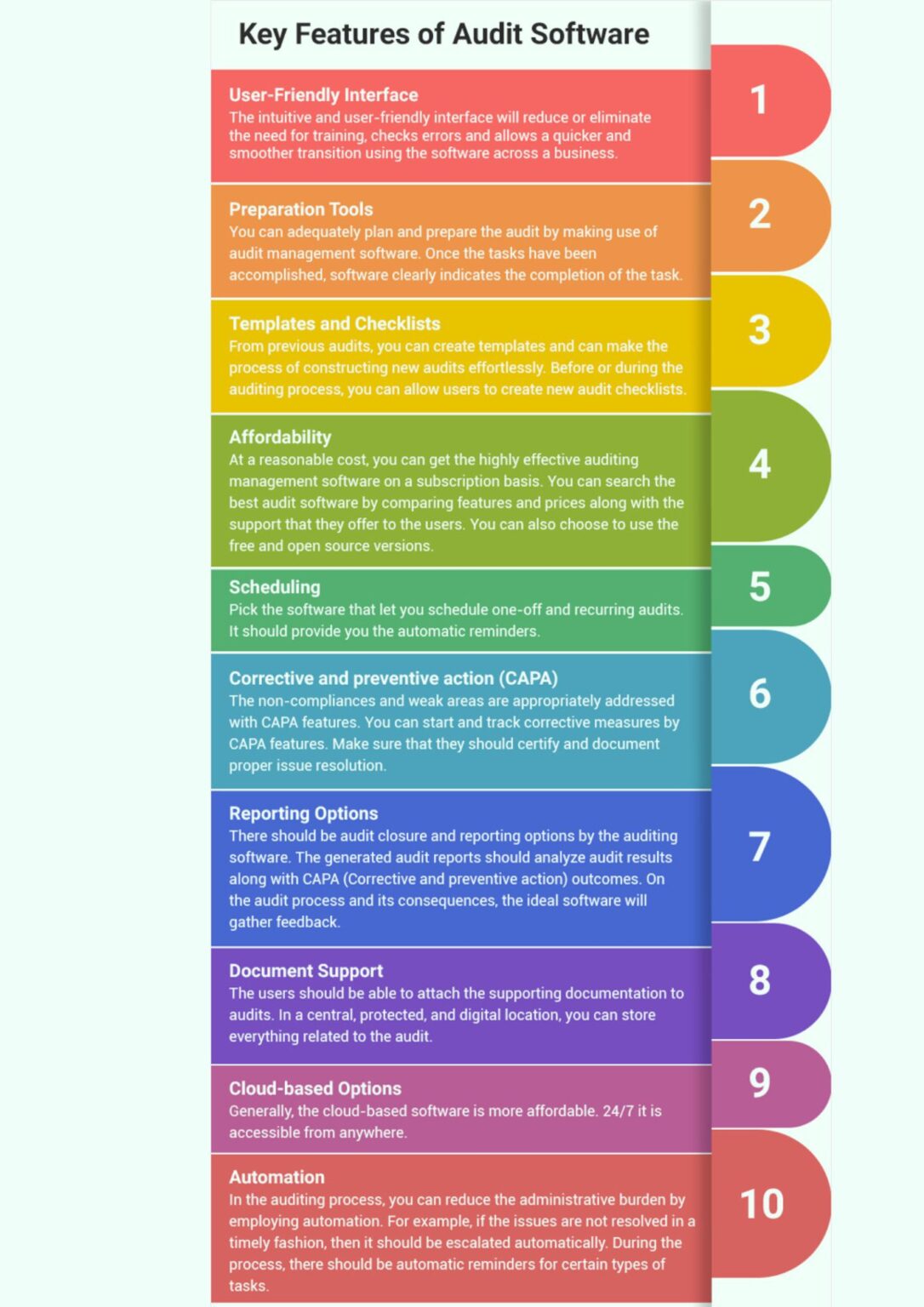
Their service was fully digital and they were using a system similar to InvictIQ for their audits, but the sister home was still paper based but thought the audit processes could be improved on. It got me thinking about how many other services across the country may not have audit processes in place or have one that is not working for the service or the manager in place, and I thought I would put together a simple 10 step-by-step guide.
Step 1: Understand the business and service needs.
Before implementing any audits, changes or processes, it is essential to understand what audits you need and the business need for them. There is no point in auditing for audit’s sake, so make sure you understand what you want from them. Is it that you want to use them to drive compliance, to enhance the quality of care or for ensuring overall oversight of your service? Or is it for something else?
Step 2: Define the audits.
Step 3: Establish a system.
Once you know the need of the audits, you will be able to start defining the audits and could be medication management, infection control, resident well-being, training, maintenance etc.
It is important that as an organisation you begin to think about the systems you want in place for auditing. Whilst there is a place for paper audits, we are seeing these quickly becoming a thing of the past, with more and more providers moving to digital offerings, with services like InvictIQ which allow you complete oversight and transparency with the auditing taking place in your service.
Step 4: Pull together a working party.
Step 5: Develop Audit Tools
This isn’t always a necessary step for small providers, but if you manage a service with different departments or heads of services, pull together a working party with representatives from each department.
During stage 4 and 5, you can begin to assign roles and responsibilities to each member of the working party and begin to develop and devise your audit tools. It is important that the audit tool is easy to understand and use.
Once the audits have been devised and you are happy with them, and its important as a Registered Manager that you are happy as it is your name with the regulator, that you begin to look at audit schedules. Digital systems will make this process smooth and timely, however you need to establish frequency of completion, timescales for actions to be rectified and lessons learnt deadlines.
Step 6: Training and upskilling.
It is important that you train your team on audits. It is not a tick box exercise, and time and thought should be put into them. You should provide clear instructions on how to conduct audits, what to look for, and how to record findings accurately.
Step 7: Conduct audits.
You now have the reason why you want the audit, the benefit it will have on the organisation, team or person being supported, and you will have staff who are upskilled and trained and know what is expected, so the next step is to conduct the audit schedule. Those that have been assigned to each audit should follow the guidance you have provided and use the tools to assess the objectives.
Step 8: Gather feedback and act accordingly.
Collect all the data and findings from the audits.
Compile the results into a structured format, highlighting areas of excellence and areas that need improvement.
Once you have identified the areas that need improvement, prioritise these based on their impact on resident care and wellbeing.
Work with relevant teams to create action plans for addressing the identified improvement areas. Assign responsibilities and set deadlines for implementing corrective actions. These actions could include staff training, policy updates, process changes, etc. It is important that you document outcomes, what has been done and lessons learnt, as this is great evidence to use in team meetings and during inspections to show continuous learning and internal improvements.
Step 9: Review and Monitor.
Regularly review the progress of the implemented corrective actions. Digital systems like InvictIQ will allow you to set reminders and some systems embed into your calendar. It is important to measure improvements and ensure that the changes are having the desired effect.
It may be during this stage that you need to adjust your strategy/correction action and this is fine. Make sure you document the reason why, again for internal learning and to evidence to the regulators and in inspections.
Step 10: Re-review, utilise the data and communicate.
Good practice would be to revisit audit objectives, tools and processes to ensure they remain relevant and effective. Incorporate feedback from staff, residents and their representatives to refine the auditing process further.
You will now be collating more data and insights than you historically had, so make sure you do not just sit on this and utilise the data to identify trends and patterns and to help you make informed decisions.
I have spoken about using findings for lessons learnt sessions with your team, but don’t forget to communicate with the people you support and their families. There will be nothing more reassuring than the transparency of you being honest about what you have found and what you have done to address the issue and will put you on the right path to increasing trust and reinforcing your commitment to high quality care which is continuously reviewed.
By following these steps, you will be able to successfully introduce audits into your care service, leading to better quality of care and an enhanced environment for the people you are supporting.
Remember that the ultimate goal is to continually improve the wellbeing, safety and satisfaction of the residents under your care.