Risk assessments are crucial to high quality care delivery but are something that I see time and time again being mentioned in CQC reports under the Caring domain of how providers are failing to support people to be independent whilst managing risks. Diving into some Registered Manager groups there are numerous comments following CQC inspections and PAMMs audits of how providers have been advised to include more detail and questions around which risk assessments are needed and for examples to get ideas of what to include.
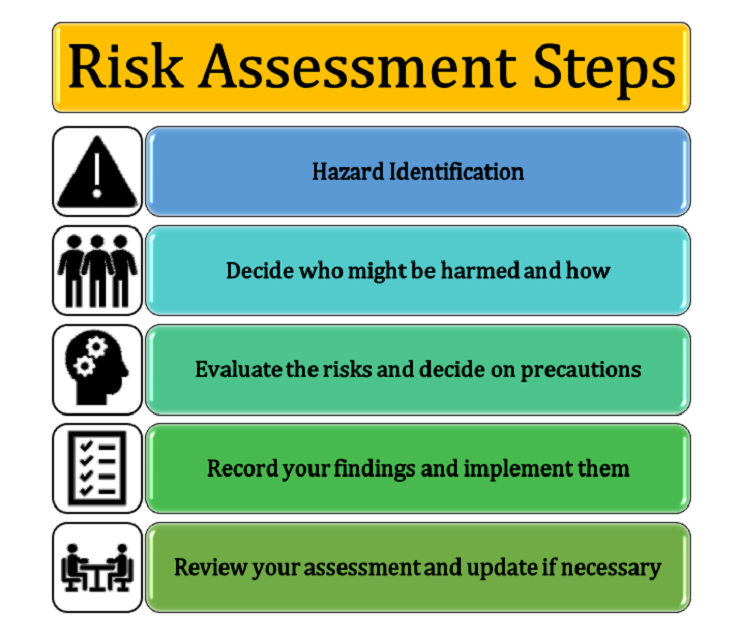
There are a number of risk assessment training courses and many templates available on the internet, however, remember that the most important things to include are sections that allow you to document the hazards, what the risks are and the potential impact, how you are controlling/reducing the risk and a section for reviewing them.
It is clear there is more emphasis on managing risk, and not only do we need to ensure we have the right template and the right detail within the risk assessment but that we also map what we are doing to each of the Quality Statements and I Statements to ensure that all potential risks are addressed within the context of achieving and evidencing high-quality care.
Taking a quick look at some of the Quality Statements, it is clear that the CQC expect:
- Providers to ensure that people receive timely care and avoid unnecessary delays
- People are protected from avoidable harm (Safe domain)
- Care to be based on evidence and achieve desired health outcomes (Effective domain)
- Providers to be responsive and respond to individual preferences, needs, and values (Responsive domain)
Steps to Map Risk Assessments to Quality Statements
Firstly, I would not advise you use the Quality Statements to produce risk assessments but rather use them as a safety net to double check you have the measures in place to keep people safe. The steps and approach I would take would be:
- Complete risk assessments for each known risk. Utilise your team, the person themselves and their representatives to inform these assessments and mitigate as many risks as possible.
- Ask someone else to double check the risk assessments. This process is a failsafe to ensure there is nothing else that could be included to mitigate the risks.
- Set time aside to go through each Quality Statement. Reflect on this statement and each of the We and I statements and think ‘have I don’t all I can do to evidence this/safeguard the person in question’. Please note that not all Quality Statements, I Statements will be applicable to managing risks.
Let’s dive into the Effective domain and the ‘Delivering evidence-based care and treatment’ Quality Statement. I have added each of the main points of the statement and the I statements with notes about how I would review this Quality Statement.
Example
Quality Statement
We plan and deliver people’s care and treatment with them, including what is important and matters to them. We do this in line with legislation and current evidence-based good practice and standards.
For this I would ensure that the care plan and risk assessments truly reflect what is important to the person, what matters to them, what they hope to achieve, what their goals are (short, medium and long term), what they need from you and your staff, what their history is, what their likes are, what they dislike, what they can and cannot do etc. Really dive into the person. From this you will be able to form the risks associated with each of the things they would like to do/achieve.
What this quality statement means
- People receive care, treatment and support that is evidence-based and in line with good practice standards.
- The provider’s systems ensure that staff are up to date with national legislation, evidence-based good practice and required standards.
- People are told about current good practice that is relevant to their care and are involved in how this is reflected in their care plan.
- People’s nutrition and hydration needs are met in line with current guidance.
- Staff and leaders are encouraged to learn about new and innovative approaches that evidence shows can improve the way their service delivers care.
In order to meet numbers 1 and 2 above, I rely on evidence-based guidance and quality standards from reputable sources like NICE and the CQC themselves. I personally subscribe to CQC and NICE newsletters to stay up to date but also utilise their websites. For NICE I use their ‘pathways’ function to find their guidance and utilise their flowcharts to help put guidance into practice.
To meet number 3, I utilise some of the NICE flowcharts, but try to breakdown guidance into bitesize pieces to cascade to my team, the people I support and their representatives. Sometimes breaking down the guidance, I find it gets my thoughts flowing and brings new ideas or thoughts to implement.
To meet number 4, I would google the point and see what comes up on google to help educate me. I can see from Google it links me to Regulation 14, various blogs and articles, NHS websites, Skills for Health and other reputable sources. It does take time to read each of these and digest them but by doing so you will get new ideas that you haven’t considered, find best practice examples and much more. It is this that will help you excel in each quality statement, deliver outstanding care and set you aside from other providers.
Number 5 is doing what I have explained in number 4, but also upskilling yourself and the leaders in your organisation through training, webinars, group forums etc.
Remember to also check the bottom of each Quality Statement webpage for Related Regulations, Additional Legislation and Best Practice Guidance. This won’t be something you can do quickly, so set time aside. Remember you have the core risk assessments to protect people and this mapping process is to check if there is anything you missed or haven’t considered.
I Statements
- I can get information and advice about my health, care and support and how I can be as well as possible – physically, mentally and emotionally.
- I have care and support that is co-ordinated, and everyone works well together and with me.
- I have care and support that enables me to live as I want to, seeing me as a unique person with skills, strengths and goals.
To meet the I Statements above I would meet with my team and the person being supported to ask these questions. Do you meet these statements, what more could you do to be compliant, what more could you do, does your team need more resources/tools to enable this to happen, are their feedback mechanisms in place etc. Asking these questions will enable you to drive positive changes into your organisation. As well as asking the question, also consider staff training, protocol adjustments or technology implementations to help meet the Quality Statement.
Which risk assessments?
There are many risk assessments when it comes to social care, and there is no definitive list. The most common ones I find are:
- Pets – remember aquatic pets come with water risks, dogs and saliva, cat faeces with pregnant workers etc.
- Managing medication independently
- Handling medication
- Environmental
- Fireworks (think about the noise and light impact as well as the health and safety risk)
- Slips, trips and falls in the office (homecare)
- Falls
- Hot Water
- Movement of objectives (office)
- Moving and Handling
- Lone working
- Christmas decorations
- COSHH – storing, using, those with capacity using their own, service owned and individual owned products
- Challenging behaviour
- Allergies
- Burns
- Choking
- Infection control
- Food handling
- Legionella
- Fire
- Asbestos
- Bedrails
- Equipment
- Staffing Levels
One thing that came out of a PAMMs inspection for one of the services I oversee, was to have a short, brief guide on what to do if a risk happened, and for the action staff need to take. I really liked this idea and thought it proved a great resource for staff who may become panicked or stressed when a risk happens. (Three sample risk assessment templates are available for free takeaway in the Infographic section.)
Audit on Cloud by InvictIQ is an excellent choice for carrying out risk assessments, offering a wide range of templates from their Digital Library. The platform’s automated Action Planning streamlines the process, making it more efficient for care providers. This combination of resources and automation ensures thorough and effective risk management.
Final Thoughts
Remember there is more emphasis on managing risk than ever before with the new Single Assessment Framework and as providers we need to ensure we have captured and mitigated all risks. Mapping to each of the Quality Statements and I Statements ensures other potential risks are addressed within the context of achieving and evidencing high-quality care.