@2021 invictIQ is a venture by Sprint Consultancy. All rights reserved. Privacy Policy.
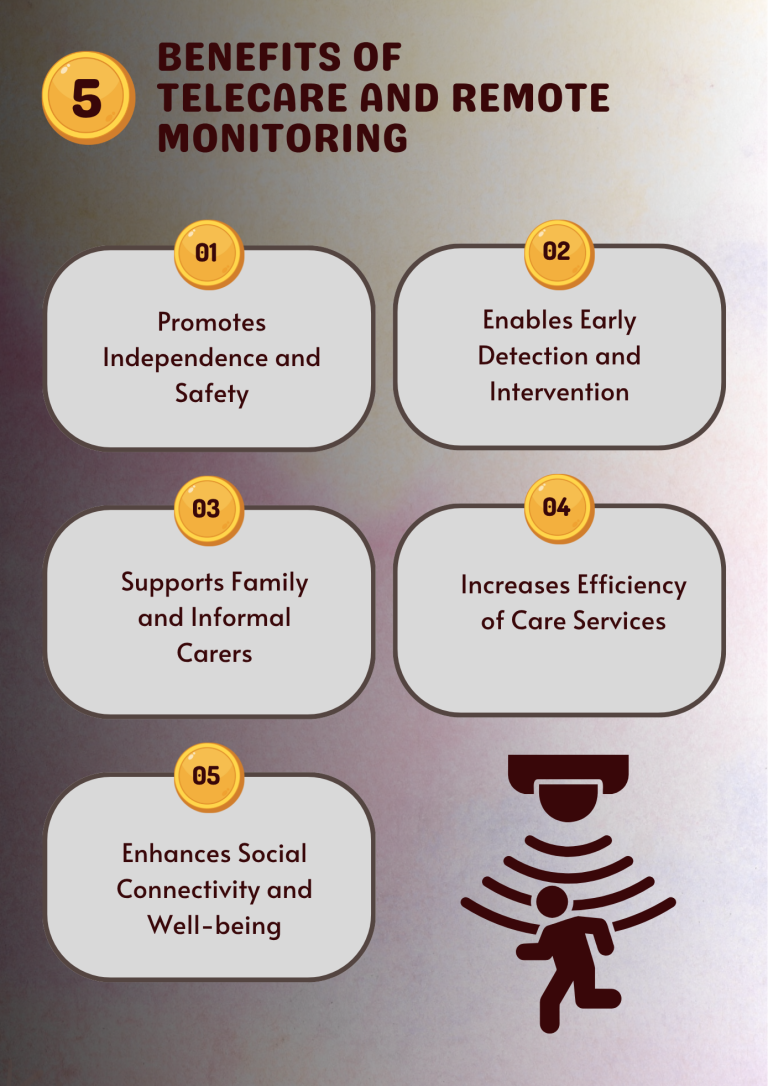
Benefits of Telecare and Remote Monitoring
by Mark Topps
Telecare and remote monitoring have quickly become everyday parts of social care packages, modernising traditional care that is provided. Studies have shown they can support better outcomes for people, reduce hospital admissions, provide unrecognised insights and provide reassurance for the person and their loved one. I recently attended the Digital Care Summit in London, and thought I would reflect on remote monitoring.
I touched on a couple of the benefits in my opening statement but it was clear from listening to speakers, especially Clare Morris, CEO of Rethink Partners that telecare and remote monitoring removes geographical barriers, enabling people in rural areas to access services without the need for travel. Some of the other benefits included:
- The ability to empower people to actively manage their health, with their family or care provider tracking vital signs, data and symptoms from home. The reports coming out of Cera Care have also shown that individuals become more engaged in their care, which ultimately improves care outcomes.
- Reduction in hospital readmissions.
- The ability to intervene more quickly based on data and trend analysis.
In the UK, providers must ensure that telehealth/telecare practices meet standards, including UK GDPR and the Data Protection Act to guarantee the lawful and transparent use of personal health data. Legislation is clear that consent must be clear, specific, opt-in, properly documented and easily withdrawn to respect individual rights so it is important that these things are thought about before rolling out any service. From an auditing and compliance point of view, it is good to continue checking consent so you know it is up to date.
One of the biggest lessons learned from my experience of some tech pilots is establishing whether you are the data controller or processor and then applying the appropriate safeguards accordingly.
Digital records should follow Professional Record Standards Body (PRSB) guidelines and I would urge providers to complete the Data Security and Protection Toolkit (DSPT) as this provides free tools and resources to support you to implement the safeguards needed and can act as an annual audit for your cyber readiness.
The last part of auditing really comes down to everything we do, and that’s the people using our services. Feedback from individuals, families and staff provides invaluable insight into what works and what doesn’t. Are platforms intuitive or are they creating frustration? Do people feel supported and connected, or does remote care feel impersonal? Gathering feedback through surveys, focus groups or informal conversations helps identify barriers such as poor connectivity or accessibility challenges and allows you to act.
Audit software like InvictIQ’s Audit on Cloud automates the collection and analysis of compliance data and feedback making it easier for providers to monitor standards and respond to issues. Most have real-time dashboards, automated alerts and historical logs so that managers and providers can track everything and ensure nothing slips through the cracks.
The success of telehealth and remote monitoring isn’t just about technology, it’s about leadership and effective change management. Introducing these tools requires a cultural shift, clear communication and strategic planning with leaders who are championing digital transformation. Remember, these tools change how many staff work, and there is a lack of digital skillset and awareness. For organisations, it’s not just about investing in the tech itself, but also the training and development of the teams using it. There are many blogs and resources on change management but do reach out to me or InvictIQ if you feel a blog on this would be of use.
As we move to a digital era, there are more questions around inclusion and equity, and telecare/telehealth options are in the same boat. Not everyone has reliable internet, a suitable device or the confidence to use technology. For some, language barriers or sensory impairments make digital platforms challenging, and for others there is a cost element. Equity in access is something we all need to strongly consider.
Telecare and remote monitoring are only the beginning of a much larger digital transformation in social care. Emerging technologies such as AI-driven analytics, predictive algorithms and wearable devices will revolutionise how we meet and respond to people’s needs. We already have tools that can predict a fall risk or a deterioration in health and allow earlier intervention, but imagine a world where tools take the next step to auto schedule an appointment, smart home technology becomes an ecosystem with healthcare systems. Digital advances are rapidly evolving as it’s the responsibility of us as leaders to shape the services we deliver and be future-ready whilst remaining person-centred.
MORE ARTICLES

Mark Topps is a social care leader who has worked in the care industry since 2004 and is currently working as a regional support manager. He regularly advocates, appearing on television, radio and podcasts and has started many campaigns for change in legislation and culture within the industry. Mark is the co-founder of The Caring View which is a social care podcast, YouTube show and free resource initiative for the sector. He also co-founded The Health and Social Care Club, which is an audio event hosted on LinkedIn. Mark is also the social media and marketing director at the National Association of Care and Support Workers.
Sign up for our newsletter