@2021 invictIQ is a venture by Sprint Consultancy. All rights reserved. Privacy Policy.


5 Social Care Compliance Risks : Must-Have Solutions
by Mark Topps
Compliance is crucial when it comes to social care, and failures can lead to large fines and possible imprisonment. There is a different regulatory body per nation of the UK. In England this is the Care Quality Commission (CQC), Scotland has the Care Inspectorate, Wales have the Healthcare Inspectorate Wales (HIW) and Ireland have The Health Information and Quality Authority (HIQA). Each have their own standards and it is important to understand what these are to ensure you remain complaint.
There are a number of compliance risks, some that are nation specific, and some that cover the whole of the United Kingdom and in this blog I dive into the top 5 that could impact across the whole of the UK and some solutions to avoid falling foul.
1.Training
Whilst guidance and legislation around training is not always clear and transparent, and could be open to interpretation, all regulatory bodies set out their minimum expectation and there should be an onus of each care provider to ensure they employ, train and upskill their workforce on a regular basis as without this there is a significant risk of poor care and an unsafe service.
To avoid this happening care providers should:
- Ensure they have a robust recruitment and onboarding process, including induction and orientation training and shadowing.
- A robust training matrix which sets out the type of training, whether it will be delivered face to face, remote or e-learning and the frequency for re-training.
- Staff feedback following training sessions, both with the trainer and a follow up.
- Robust policies for whistleblowing, complaints and for the actions to be taken following poor practice (such as re-training, shadowing etc)
- Regularly supervisions.
- In the field observations and competence checks.
- Peer to peer training/upskilling.
- Individual development and career pathway plans.
- Reading corners in the office/service with resources, guides, books etc.
- Regular staff meetings.
2. Medication Management
Medication management is a complex but essential component on delivering high quality care and keeping people who use our services safe and well. Proper medication management involved adhering to strict regulations and procedures to ensure people receive their medication at the right time. Failure to manage medications effectively can lead to severe consequences, both for the person receiving care, the care worker and for the reputation and trust of the organisation. Here are some steps to mitigate the risk of getting it wrong:
- Staff should receive medication training as part of their induction. This should be following be competency assessments and signing staff off before they deliver medication independently.
- Staff should have regular, un-announced medication competency checks.
- Poor practice should be addressed immediately and actions put in place for re-training/upskilling.
- Robust policies for whistleblowing, duty of candour and medication management.
- Providers should strive for a culture of learning instead of blame and punishment, so that people feel confident of coming forward when making a mistake.
- Care plans should be clearly documented with medication support needs.
- Records should be checked to ensure they are clear, accurate and reflective of the support people have provided.
- Regular audits of medication administration records should be undertaken to highlight any errors and so remedial action can be taken.
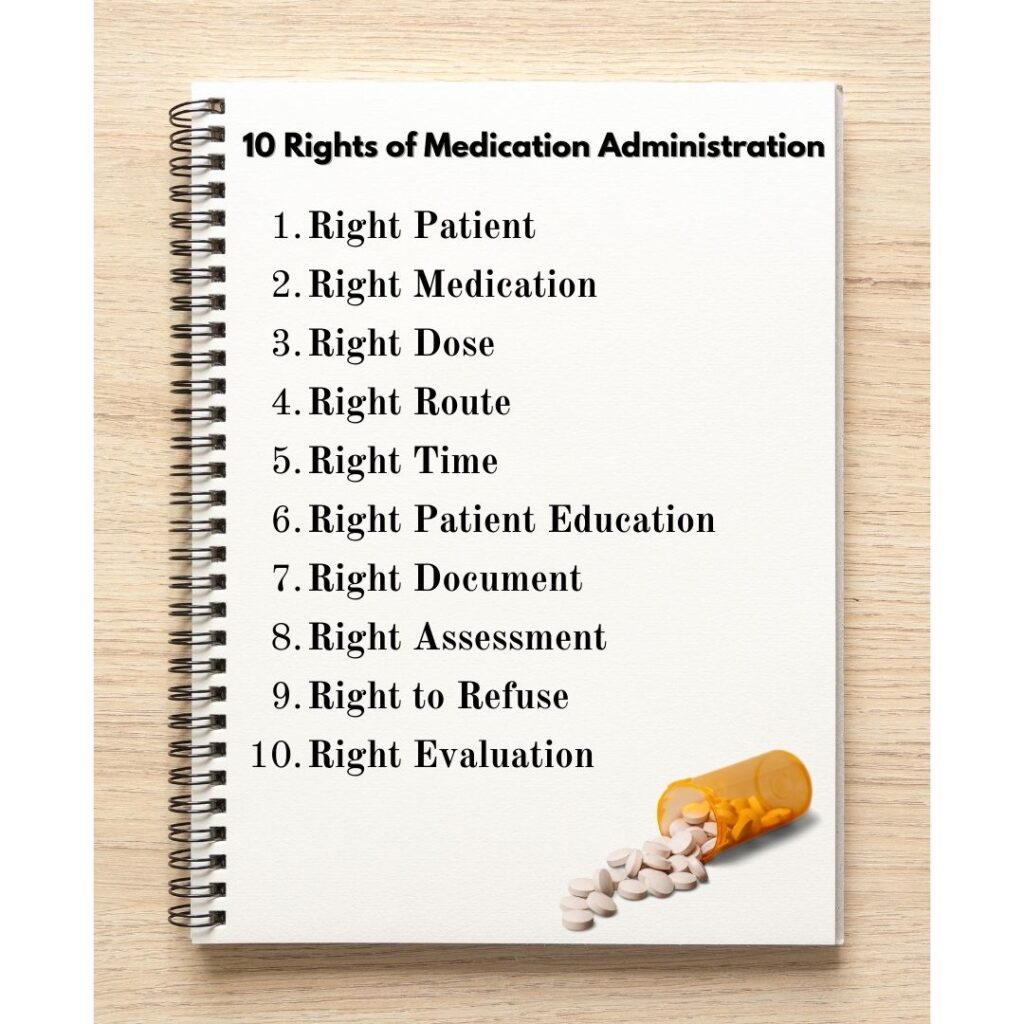
- Medication rooms/areas should have best practice guidance. Whilst we have the 5 rights of medication, some are trained in the 6 rights, and I found this insightful guide from Nursing Notes which could be interpretated for social care providers and their services.
- Team meetings should discuss lessons learnt from medication errors.
- Ask the local pharmacy to undertake an audit of your medication and records.
- Upskill team members to be medication champions.
- Ensure staff have access to the BNF (either physical or the app on their phones)
- Have clear guidance on what to do if there are medication errors.
3. Data Protection and Privacy
Data protection and privacy are paramount, and providers have a duty of care to their teams and the people they support. In the UK, all companies are governed by the General Data Protection Regulation (GDPR), which sets stringent standards for the handling of personal data. Here are some tips to remain compliant:
- Consent
- Documented clearly in each section of the care plan.
- Before care is delivered.
- During the onboarding and induction process for staff
- Regularly reviewed.
- Before sharing records.
- Clearly communicated about how to withdraw.
- Create and maintain a comprehensive GDPR policies, that contains:
- Introduction
- Definitions
- Principles for processing personal data
- Types of personal data you process.
- How you will process personal data
- Legal Basis
- Retention of personal data
- Who you will share personal data with
- International transfers of personal data
- Data rights
- Changes to your privacy policy
- Undertake the Data Security and Protection Toolkit (DSPT) which will help ensure you have measures in place to remain safe and secure online.
- Data security measures such as:
- Paper records are kept in locked filing cabinets.
- Electronic devices should be encrypted.
- Access control measures to ensure data is only viewed on a need to know basis.
- Staff should be trained in privacy/GDPR.
- There should be a Data Protection Officer (DPO).
- Confidential waste bins should be in place.
- Devices should be password protected, and where possible this should include two-factor authentication.
- Data drills to check and the organisation would respond to a data breach, lack of internet etc.
4. Health and Safety
I feel like we are upskilled in health and safety more than any of us would like, but it is such a high risk and important item that I could not leave it outside of the top 5. All organisations are responsible for their staff under the Health and Safety at Work Act 1974 and have a duty of care to the people they support and those who come into contact with the organisation. Some things to ensure you have in place to remain compliant include:
- Workplace risk assessments
- Office
- Adults’ individual homes
- External risk assessments
- Checks to ensure equipment is safe for use and regularly inspected.
- Staff should be trained as part of their induction training and on a regular basis on Health and Safety, Moving and Handling, Infection Control and Hygiene Practices.
- Team meetings should contact a dedicated health and safety section on the agenda.
- Staff should have regularly, un-announced observations to ensure compliance.
- Accident and Incidents should be reported and shortcomings addressed.
- Lessons learnt should be shared across the organisation.
- Audits for Health and Safety, First Aid Box checks, Infection Control should be in place. Platforms like audIT On Cloud by InvictIQ come handy for seamless audit and inspections. With their adaptive AI backed automated features, conducting error free inspections are super easy.
- A clear and accessible health and safety policy and risk assessments.
- Upskill team members to be health and safety, infection control, hygiene champions.
- Ensure you display a health and safety poster, with up to date contact details.
- Ensure accident records are easily accessible and utilised.
- Ensure first aid provision:
- First aid boxes
- If community based, individual first aid packs.
- Contingency plans in place and regularly tested.
5. Record Keeping and Documentation
We have that famous saying in social care ‘if it isn’t documented, it didn’t happen.’ Here are some things to ensure you remain compliant:
- Induction programmes should contain accurate record keeping and highlight best practice and expectations. Remember, some organisations may not have as high a standard as you do.
- Remind staff not to use abbreviations, COT may not mean cup of tea for everyone.
- Spot check staff records to ensure they are legible, clear, detailed, signed and dated.
- Look at standardising forms and templates for consistent documentation.
- Look at best practice guides to help staff complete records, care notes and documents.
- If you are a paper-based service, look at implementing a secure electronic record keeping system and/or audit system. audIT on Cloud by InvictIQ ensures a single source of truth with all actions, evidence and reports centralised in the cloud and easily retrievable. With real-time data insights for effective storytelling, it ensures your Care business is compliance ready always.
Final thoughts:
Compliance is something that we cannot move down our to do list, but something that needs to be prioritised and continuously reviewed. Non-compliance poses a risk to the well-being of those we support, lead to regulatory scrutiny, financial penalties and damage to a provider’s reputation.


Mark Topps is a social care leader who has worked in the care industry since 2004 and is currently working as a regional support manager. He regularly advocates, appearing on television, radio and podcasts and has started many campaigns for change in legislation and culture within the industry. Mark is the co-founder of The Caring View which is a social care podcast, YouTube show and free resource initiative for the sector. He also co-founded The Health and Social Care Club, which is an audio event hosted on LinkedIn. Mark is also the social media and marketing director at the National Association of Care and Support Workers.
Share
Sign up for our newsletter